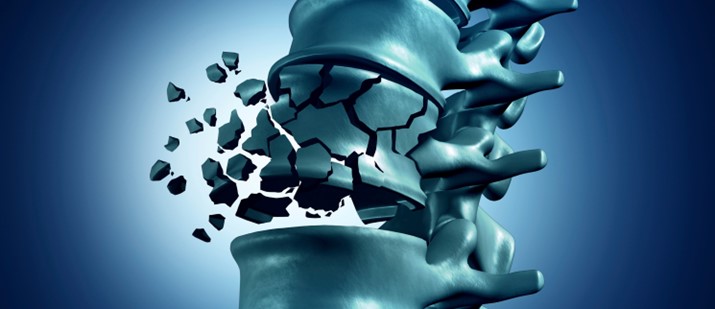
Suffering a fracture late in life can be a sentinel moment for a person. Pain from the injury is not the only problematic consequence. The one year mortality in elderly patients suffering a hip fracture can be as high as 20%. Hip fractures result in decreased mobility and increased incidence of deep venous thromboses. Vertebral fractures can lead to decreased thoracic and abdominal volume, impaired pulmonary function, and digestive problems. Finally, fractures have been linked to depression in the elderly.
Osteoporosis
Suffering a fracture late in life can be a sentinel moment for a person. Pain from the injury is not the only problematic consequence. The one year mortality in elderly patients suffering a hip fracture can be as high as 20%. Hip fractures result in decreased mobility and increased incidence of deep venous thromboses. Vertebral fractures can lead to decreased thoracic and abdominal volume, impaired pulmonary function, and digestive problems. Finally, fractures have been linked to depression in the elderly. The correlation between fractures and low bone mineral density (BMD) is well documented. Osteoporosis, which is defined by the World Health Organization as BMD 2.5 standard deviations or more below the mean peak bone mass of young, healthy adults, is estimated to affect over 200 million people worldwide. Approximately 30% of all postmenopausal women have osteoporosis in the United States and in Europe. At least 40% of these women and 15-30% of men will sustain one or more fragility fractures in their remaining lifetime.
Bone is a dynamic substance composed of two distinct structural elements. Trabecular bone is the system of rods and plates within the central cavity of bone which provides the primary resistance to compressive and tensile forces. Cortical bone is the thicker bone which surrounds the inner trabeculae. Both components of bone constantly remodel, but the rate of bone turnover in trabecular bone is greater than in cortical bone. Consequently, when women go through menopause, there is increased loss of bone in areas of predominantly trabecular bone such as vertebrae, the proximal femur, and the distal forearm. It should come as no surprise, then, that these are areas prone to osteoporotic fractures.
A substantial risk factor for the development of osteoporosis is a low lifetime peak BMD. Unfortunately, a person typically attain their peak bone mass in the fourth decade of life. After that, BMD steadily declines. In women, bone loss rapidly declines after menopause. For these reasons, medical therapy is often necessary to treat osteoporosis and prevent potentially devastating fractures.
Therapy
The historical mainstay of osteoporosis therapy in women was hormone replacement therapy (HRT). This was shown to prevent postmenopausal bone loss, and there was evidence that HRT reduced the incidence of osteoporotic fractures. However, the Women’s Health Initiative Study (2002) found that these benefits came at the unacceptable increased risk of thromboembolic disease, stroke, coronary artery disease, and breast cancer. An alternative to traditional HRT are selective estrogen receptor modulators (SERMs). These drugs are agonists for the positive bone preservation effects of estrogen while being antagonists for the stimulation of breast and uterine tissue. SERMs may also have cardiovascular benefits. Studies have shown one SERM, raloxifene, to decrease the risk of vertebral fractures with the side effect of increased incidence of thromboembolic disease.
Other osteoporosis therapy can be lumped into two broad categories: drugs that inhibit the resorption of bone and drugs that attempt to build BMD. Bisphosphonates are the crux of the former group. These drugs are stable analogs of inorganic pyrophosphates which bind to bone and decrease its turnover. Bisphosphonates are currently available in daily, weekly, and monthly oral preparations as well as quarterly parenteral formulations. Patients occasionally have problems complying with the administration regimen of oral bisphosphonates which requires the medication be taken on an empty stomach with a full glass of water while remaining upright for 30-60 minutes before eating. All bisphosphonates have been shown to decrease vertebral body fractures but not all have been shown to decrease non-vertebral osteoporotic fractures.
The latter therapy group, drugs attempting to build BMD, presently includes calcium and vitamin D and recombinant parathyroid hormone. As stated previously, a person attains his or her peak bone mass in the fourth decade of life. Hence, the benefit of calcium and vitamin D later in life is controversial. Regardless, many consider these an important adjunct to other osteoporosis therapy. Recombinant parathyroid hormone is given as daily subcutaneous injections and directly stimulates osteoblast function. A study of this medication showed it to increase BMD and decrease the risk of vertebral fracture. The high cost of this medication restricts its use to patients with severe osteoporosis and high risk of fracture.
No osteoporosis therapy is perfect, and clinical trials are ongoing in search of better drugs to treat this disease. The characteristics of a model therapy are complex. There are predictable ideal features such as ease of administration, low side effect profile, and cost effectiveness. Less straightforward is determining how efficacious a therapy is: how well it increases BMD and prevents fractures.
Dual X-Ray Absorptiometry (DXA)
BMD can be measured many ways. Some of these, such as biopsy, are invasive; however, non-invasive alternatives such as dual x-ray absorptiometry (DXA) and quantitative computed tomography are more practical for screening the typical patient population.
DXA has been the standard means of Osteoporosis diagnosis for years. This procedure involves passing photons of two different energies through a patient. An algorithm uses the disparate transmission through the patient to calculate BMD. This is inexpensive, rapid, uses a low amount of ionizing radiation, and, if performed on the same system, is highly reproducible. DXA is also widely available in the clinical setting.
While these features of DXA make it useful in daily practice, there are potential problems with using DXA for measuring BMD in clinical trials. Most conventional DXA scanners only examine the anteroposterior projection. Density measurements are confounded by artifacts like degenerative endplate remodeling and spurring, overlying atherosclerotic disease, and implantable devices as well as the normal posterior vertebral body elements which erroneously increase measured BMD. In addition, DXA measures total BMD and does not distinguish between trabecular and cortical bone.
DXA also lacks the sensitivity to detect small changes in BMD which is frequently important in a clinical trial investigating drug efficacy. When using the same DXA equipment on the same patient, the 95% confidence interval for BMD measurement is approximately 2.8%. Since the mean annual increase in lumbar spine BMD with bisphosphonate therapy is approximately 3%, following therapy in clinical trials with DXA cannot usefully be performed more often than once a year.
Quantitative Computed Tomography (QCT) A more sensitive and often more specific tool for measuring BMD in clinical trials is quantitative computed tomography (QCT). Using widely available scanning techniques combined with specialized software, QCT analysis performed in the core lab provides separate estimates of trabecular and cortical BMD as true volumetric mineral density in milligrams per cubic centimeter. These values are not confounded by adjacent structures and may be separated into definite anatomic sites, including peripheral bones as well as vertebrae. As with DXA, QCT results can be expressed as T-scores and Z-scores relative to healthy young and age-matched adults, respectively. QCT has been shown to predict vertebral fractures with greater sensitivity than DXA because it selectively assesses the most metabolically active trabecular bone in the center of the vertebral body. Dual energy techniques available on higher end CT scanners further enhance the specificity of BMD measurements by QCT. The additional information from two photon energies is utilized to distinguish better between red and yellow marrow elements amid the trabeculae, achieving even more accurate BMD measurements.
The CT data used in QCT calculation also potentially increases the sensitivity of fracture detection: the ultimate end-point in determining osteoporosis drug efficacy. Morphometry is the process by which anatomic calculations are used to identify early fractures which are undetectable by radiography and DXA.
Finally, structural factors in osteoporosis, such as bone architecture deterioration, contribute to overall fracture risk independent of BMD. Image analysis allows radiologists to monitor these physical characteristics of bone in a clinical trial as well. MicroCT can achieve a resolution as small as 6 micrometers to assess improvements in bone microarchitecture which may result from osteoporosis therapy. In the near future, high resolution magnetic resonance imaging (MRI) may also be able to detect subtle alterations in bone construction without the need for ionizing radiation.
Summary
In summary, osteoporotic fractures can be devastating. There are challenges to finding an optimal treatment for osteoporosis. As clinical trials search for a novel therapy, selecting precise methods for monitoring the efficacy of new drugs using noninvasive imaging is a vital aspect of any trial.
Volume 4, Issue 11: Guidance For Sponsors: Osteoporosis Therapy – Challenges in Monitoring Efficacy in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.